If you feel as though you’ve slept 7-9 hours and you don’t have any sleep disorders or it is under control but still drowsy the next day, sound could be a possible reason.
While you sleep, your brain continues to register and process sounds on a basic level. Noise causes you to wake up, move, shift between stages of sleep, or experience a change in heart rate and blood pressure so briefly that you don’t remember the next morning. Noises are more likely to wake you from a light sleep (stages 1 and 2), than from a deep sleep (stages 3 and 4), and tend to be more disruptive in the second half of the night.
A few interesting facts are:
- “sound sleepers” have characteristic brain activity that may make them more impervious to noise
- Whether or not a sound bothers your sleep depends in part on that sound’s personal meaning; that’s why mothers wake up easier to a baby’s noise but may sleep through a fire truck siren.
- Studies have suggested that long-term exposure to intense noise pollution could be associated with hypertension.
The solution is to use a white noise machine, fan, or air purifier to create a background hum and block unwanted outside noise. Earplugs also work well for some people.
White noise works by reducing the difference between background sounds and a “peak” sound, like a fire truck siren, giving you a better chance to sleep through it undisturbed. If someone has difficulty falling asleep or staying asleep and doesn’t have insomnia, creating a constant ambient sound could help mask activity from inside and outside the house. There is a white noise machine that is made for this purpose. Nevertheless, the sound from TV is not considered white noise, since unlike white noise, TV sounds are constantly changing in tone, volume, and so forth. TV can be especially bothersome if you need to wake up to turn it off and resettle into bed.
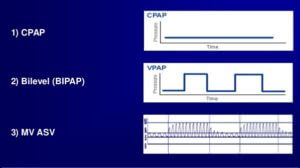
For our CanSleep CPAP users, remember as Clete A. Kushida, director of the Stanford Center for Human Sleep Research, puts it “This is why the majority of bed partners prefer the constant white noise of a CPAP machine rather than their spouse’s crescendo-decrescendo snoring sound.”
By Bahareh Ezzati (BSc, CPhT, RRT)